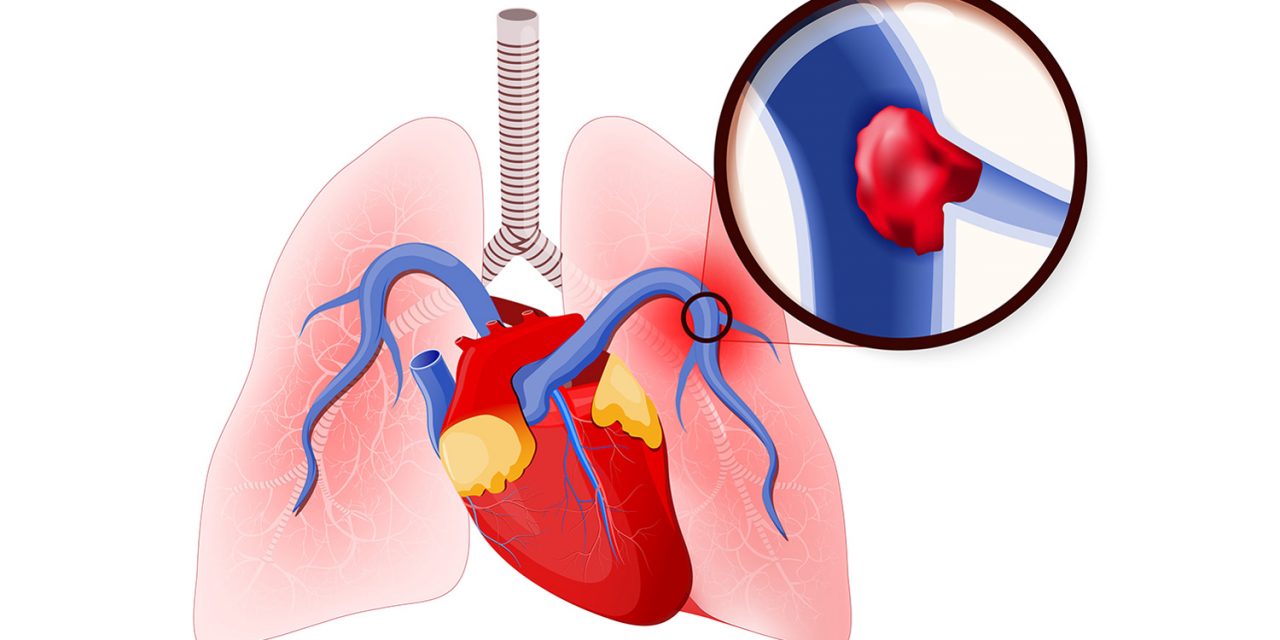
A pulmonary embolism is a blockage in the pulmonary artery, which supplies the blood to the lungs. It is one of the most common cardiovascular diseases.
Pulmonary embolism affects about 1 in 1,000 people every year in India. The obstruction, usually a blood clot, prevents oxygen from reaching the lung tissue. This means that it can be fatal. The word “embolism” comes from the Greek émbolos, meaning “stopper” or “plug.” In a pulmonary embolism, the embolus is formed in one part of the body, the whole. The blood supply seeps into it, and then it stops blood flow through the lungs to another part of the body. An embolus is different from a thrombus, which forms and stays in one place.
Symptoms
Symptoms of pulmonary embolism include:
- Chest pain, a sharp, stabbing pain that might become worse when breathing increased or irregular heartbeat
- Dizziness
- Difficulty catching breath, which may develop either suddenly or overtime
- Rapid breathing
- A cough, normally dry but possibly with blood, or blood and mucus.
Causes
A pulmonary embolism occurs when an embolus, usually a blood clot, blocks the blood flow through an artery that feeds the lungs. A blood clot may begin in an arm or leg. Known as deep venous thrombosis (DVT). After that, it is freed and travels through the circulatory system towards the lungs. There, the passage through small vessels is very large, so it creates a blockage. This blockage prevents blood from flowing to one part of the lung. This causes the affected part of the lung to die due to a lack of oxygen. Rarely, a pulmonary embolism may arise from an embolus that is formed from droplets of fat, amniotic fluid, or some other particle that enters the bloodstream.
Treatment
The first step in the treatment of most embolism is to provide shock treatment and oxygen therapy. Anticoagulant drugs, such as heparin, enoxaparin, or warfarin, are usually given to thin the blood and prevent further clotting. Required, they should be treated with an anticoagulant management service, not their primary care physician. Drug clots called ticks-break can also be administered. However, they carry the risk of excessive bleeding. Thrombolytics include actives, retavas, and aminase. If the patient has low blood pressure, dopamine can be given to increase the pressure. The patient will usually have to take medication regularly for an indefinite amount of time, usually at least 3 months.
Prevention
A number of measures can reduce the risk of a pulmonary embolism.
A high-risk patient may use anticoagulant drugs such as heparin or warfarin.
Compression of the legs is possible, using anti-embolism compression stockings or pneumatic compression. An inflatable sleeve, glove, or boot holds the affected area and increases the pressure when required.
Compression methods prevent blood clots by accumulating blood in the deep veins and reducing the amount of blood that has accumulated. Other methods of reducing risk include physical activity, regular exercise, a healthy diet, and quitting smoking or tobacco consumption.
Diagnosis
To reach a diagnosis, the doctor will look at the patient’s history and consider whether an embolism is likely. They will carry out a physical examination. Diagnosis can be challenging because other conditions have similar symptoms.
Tests for diagnosing pulmonary embolism include:
- A mathematical model that helps a doctor predict the course of DVT and the risk of an embolism
- D-Dimer test, a blood test that can diagnose thrombosis that can rule out further testing if it produces a negative result
- Pulmonary V/Q scan, two tests that analyze the ventilation and structural properties of the lungs and give off less radiation than a CT
- Computerized tomography (CT) scan, which can reveal abnormalities in the chest, brain, and other organs, and in cases where a V/Q is not possible
- Electrocardiogram (EKG), to record the electrical activity of the heart
- Arterial blood gas study, to measure oxygen, carbon dioxide, and other gases in the blood
- Chest X-rays, to generate a picture of the heart, lungs, and other internal organs
- Ultrasound of the legs, to measure the speed of blood flow velocity and any changes
- Pulmonary angiogram, to reveal blood clots in the lungs
- Magnetic resonance imaging (MRI), to obtain detailed pictures of internal structures.
Risk Factors
The risk of developing pulmonary embolism increases with age. People who have conditions or diseases that increase the risk of blood clots are more likely to develop a pulmonary embolism. A person is at greater risk of a pulmonary embolism if they have a leg or arm (DVT). ) Have a blood clot, or if they have had a pulmonary embolism in the past. Prolonged bed rest or inactivity increases the risk of DVT and therefore A, there is an increased risk of pulmonary embolism. It can be a long flight or a car ride. When we don’t move much, our blood accumulates in the lower parts of our body. If the blood is circulating less than normal, the blood clot is more likely to form. Damaged blood vessels also increase the risk. This may be due to injury or surgery. If a blood vessel is damaged, the blood vessel can become narrower, increasing the chances of blood clots forming. Other factor risks include some cancers, inflammatory bowel disease, obesity, pacemakers, intravenous catheters, pregnancy, Estrogen supplements, family history of blood clots and smoking.
32 Comments
zprГЎvy
flibanserin 0.3mg
Great post. I was checking continuously this weblog and I’m inspired! Very useful info particularly the closing part 🙂 I care for such info much. I was looking for this particular info for a very long time. Thank you and best of luck.
nimotop
Hello dratulkasliwal.in webmaster, Keep the good content coming!
luvox medication
indocin 10mg
tato strГЎnka
Great, thanks for sharing this blog post.Really looking forward to read more. Really Great.
allopurinol 300 mg pharmacy
To the dratulkasliwal.in webmaster, You always provide helpful information.
amaryl 40mg
doxycycline 100mg
floxin 20mg
To the dratulkasliwal.in owner, Excellent work!
aristocort 150mg
speciell info
What is Alpha Tonic? Alpha Tonic stands as a natural health supplement designed to comprehensively address men’s overall well-being.
mais informações aqui
FitSpresso is a natural weight loss supplement that will help you maintain healthy body weight without having to deprive your body of your favorite food or take up exhausting workout routines.
aciphex 100mg
Very interesting details you have mentioned, thankyou for putting up.
An interesting discussion is worth comment. I think that you should write more on this topic, it might not be a taboo subject but generally people are not enough to speak on such topics. To the next. Cheers
coreg 60mg
pepcid 100mg
meer informatie
You could definitely see your expertise in the paintings you write. The sector hopes for more passionate writers such as you who aren’t afraid to say how they believe. At all times go after your heart.
fonte
Super-Duper site! I am loving it!! Will be back later to read some more. I am taking your feeds also
I’d must test with you here. Which is not something I normally do! I get pleasure from reading a submit that can make folks think. Additionally, thanks for allowing me to remark!
I dugg some of you post as I cogitated they were very useful handy
There is obviously a bundle to know about this. I consider you made certain nice points in features also.